The latest research data indicate that, from 2023 to 2024, the cervical cancer screening rate among women aged 35–64 in China reached 51.5%, successfully meeting the national target of achieving a 50% screening rate by 2025. As a crucial method for cervical cancer screening, Liquid-Based Cytology (LBC) can effectively detect cervical cancer and its precursor lesions. However, a certain proportion of false negatives persists in clinical practice. The entire diagnostic process of cervical LBC, including sample collection, slide preparation, and diagnosis, contains corresponding steps that contribute to false negative results. This paper attempts to analyze the causes contributing to false negatives in cervical Liquid-Based Cytology.
① Sexual Intercourse within 24 Hours Prior to Sampling
Sexual intercourse within 24 hours prior to sampling leads to an increase in microorganisms, such as bacteria, within the vagina and cervix. This results in a rapid surge in inflammatory cells and increased mucus secretion. Furthermore, cervical friction may cause bleeding. During sample collection, the inflammatory cells and blood cells adhere to the cervical surface, making it difficult to collect cells with diagnostic value, thereby resulting in false negatives.
② Use of Vaginal Suppositories or Douches within 24–48 Hours Before Sampling
Sampling may be contaminated with drug crystals, rendering cell morphology unrecognizable and consequently leading to false negatives.
③ Sampling During Menstrual Period
The presence of a large number of blood cells in the sample collection causes interference during slide examination, leading to false negatives.
① Inadequate Exposure of the Cervix
The squamocolumnar junction (SCJ) zone is the common site for cervical lesions. Although the number of squamous epithelial cells collected may be sufficient, failure to sample this specific region can still lead to false negatives.
② Insufficient Sampling Force
The sampling head of the cervical collection device requires a certain amount of pressure to fully deploy. Some clinicians may use a gentler technique out of concern for causing bleeding during the procedure, resulting in a failure to collect the lesional cells, thereby leading to false negatives.
③ Lesions Located Deeply
If the lesional area is located too deep from the cervical os (opening), the sampling brush may be unable to reach that site.
① Impact of Sample Volume
If the volume of sample transfer during slide preparation is not adjusted according to the cell concentration, it may result in an excessively high density of diagnostic cells. These cells, being overlapping, are difficult to observe after staining, thus leading to false negatives.
② Vortexing Prior to Slide Preparation
Failure to adequately vortex/shake the vial before slide preparation may lead to incomplete cell elution from the cervical brush or insufficient dispersal of mucus, which can also result in false negatives.
③ Failure to Fix Promptly After Preparation or Using Air-Drying
Delayed fixation can cause the smear to dry out, leading to cellular degeneration. Additionally, air-drying (or dry fixation) can compromise the fine nuclear structure, making it impossible to evaluate. Both scenarios may lead to false negatives.
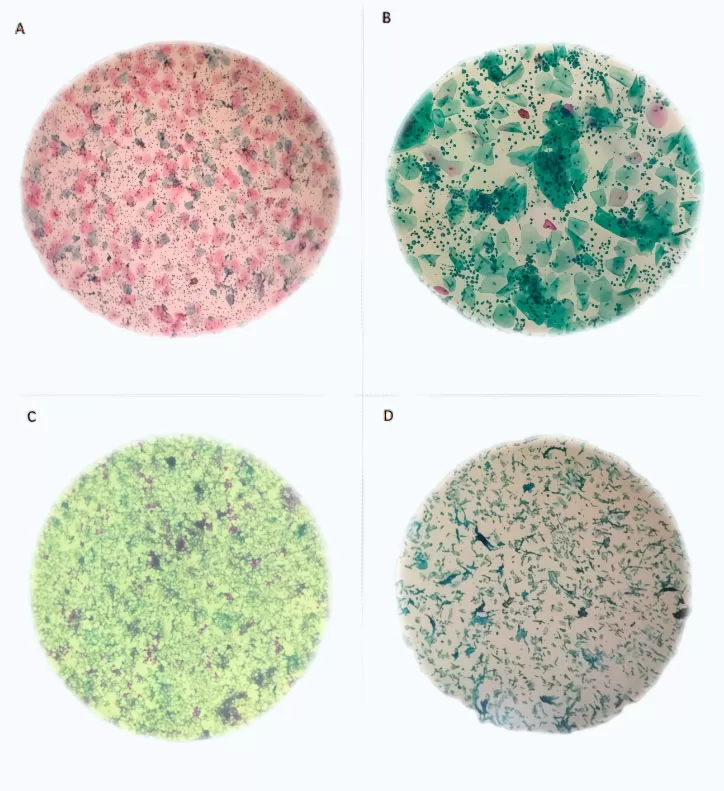
Note 1:A. Excessive inflammatory cells; B. Cellular overlapping; C. Excessive blood cells; D. Air-drying
Cytotechnologists may fail to perform an adequate evaluation of the entire slide, or their limited screening experience may prevent a correct diagnosis. Additionally, a heavy workload, resulting in visual fatigue from reviewing too many slides, can lead to missed diagnoses.
In summary, numerous factors contribute to false negatives in cervical Liquid-Based Cytology (LBC). However, with the development of LBC slide preparation automation technology and liquid based cytology technique, the application of Artificial Intelligence (AI) assisted screening, the strengthening of training for screening personnel, and the implementation of robust quality control (QC), the occurrence of false negatives in cervical LBC is expected to steadily decline.
References:
【1】 Mei Zhang, Limin Wang, et al. Cervical Cancer Screening Rates Among Chinese Women— China, 2023–2024[J].China CDC Weekly, 2025,7(10):321-326.
【2】 Wang SY, Liang HR. Analysis of Causes of False Negatives in Cervical Cytology Examination [J]. Traditional Chinese Medicine and Ethnomedicine, 2012: 67-69.
【3】 Tang HP, Hu YF, et al. Analysis of False Negatives and False Positives in Liquid-Based Cytology Diagnosis of Cervical Intraepithelial Neoplasia [J]. China Practical Medicine, 2017, (32): 58-59.
【4】 Tu DY. Analysis of Clinicopathological Characteristics of Missed Lesions in Cervical Cancer Screening by TCT [D]. Chongqing: The Second Affiliated Hospital of Chongqing Medical University. 2021: 1.
【5】 Wang J, Wang H, et al. A Prospective Study on Influencing Factors of Clinical Sampling for Cervical Cytology Examination [J]. Chinese Journal of Woman and Child Health Research, 2019, 34(2): 261-263.
【6】 Hu J, Duan YL. Investigation of False Negative Results in Cervical/Vaginal Liquid-Based Cytology and Analysis of Related Factors [J]. Preventive Medicine, 2024, 9(3): 105-107.