In routine Liquid-Based Cytology (LBC) testing, what does a diagnosis of "LSIL" on a TBS report (The Bethesda System) signify? How should it be interpreted accurately? Today, we will provide an accessible yet in-depth discussion on the key points for interpreting Low-Grade Squamous Intraepithelial Lesion (LSIL).
When HPV infection occurs in the basal layer squamous epithelial cells of the transformation zone, the virus exists in the host cell nucleus in two states: the episomal state (free state) and the integrated state. Essentially, LSIL corresponds to the episomal state of the virus. It signifies that the virus is replicating within the cell nucleus and has caused morphological changes to the cell, but the lesion is mostly confined to the lower one-third of the cervical epithelium, classifying it as a "mild" abnormality.
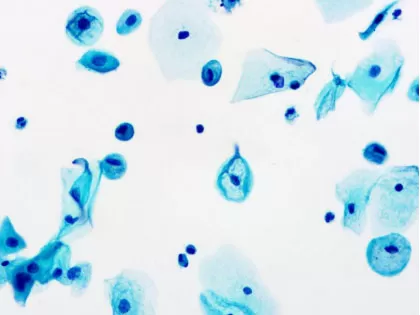
To accurately interpret LSIL, focus on the following core characteristics:
A. Nuclear Changes (Core Diagnostic Basis)
① Nuclear Enlargement:
The nuclear area is approximately three times or more than that of a normal intermediate squamous cell nucleus.
② Hyperchromasia and Coarse Chromatin:
The nucleus exhibits darker staining, and the chromatin may appear coarse or granular, but the distribution generally remains uniform.
③ Mild Nuclear Membrane Irregularity:
The nuclear membrane may show slight unevenness or undulation, but typically lacks the high degree of irregularity or nuclear grooves seen in higher-grade lesions.
④ Binucleation or Multinucleation:
This is a very common feature of LSIL and is one of the classic manifestations of HPV infection.
B. Cytoplasmic Changes (Ancillary Features)
① Koilocytes:
This is the hallmark characteristic of LSIL. It presents as a clear, halo-like zone around the nucleus (perinuclear clearing), while the peripheral cytoplasm becomes dense and thickened.
② Cytoplasmic Maturation:
Despite the nuclear abnormalities, the cytoplasm usually remains abundant and mature. This is a crucial distinguishing point from HSIL (High-Grade Lesion).
Figure 1. Typical LSIL image

Note: The slides were prepared using the HealthSky SCTW-2400A SCT method and cytology equipmentmet, and the slides were read using HealthSky Patho.P AI-assisted diagnostic technology.
In actual practice, not all LSIL cases are "typical." The following challenging patterns require special attention:
① Atypical "Koilocytes"
Some inflammation or other conditions may also cause perinuclear clearing, but the nucleus lacks atypia (only showing pyknosis). Such cases should not be interpreted as LSIL.
Figure 2: Pseudo-Koilocytes (Caused by Glycogenolysis)
② Keratinizing Squamous Cells
Parakeratosis may appear in the background of lesions associated with HPV infection. It is essential to actively look for the typical cytological changes related to HPV-induced cellular interference.
③ Interference from Slide Preparation Factors
Factors such as excessive cell thickness, inadequate fixation, or staining that is too dark or too light can all compromise the accuracy of interpretation.
Currently, for patients whose cytology reports indicate LSIL, colposcopy and cervical biopsy are universally recommended. If the histopathology diagnosis confirms LSIL, treatment is generally not required in principle, and clinical observation is sufficient. Given the high rate of spontaneous regression of LSIL, especially in young women, p16/Ki-67 dual-staining technology—as recommended by current guidelines—may be used for triage. If the dual-staining result is positive, the patient requires immediate referral for colposcopy.
Mastering the interpretation essentials of LSIL is a fundamental skill for every cytopathologist and laboratory technician. By remembering the core "nuclear" features, recognizing challenging patterns, and combining this with high-quality slide preparation techniques, we can provide clinicians with more reliable and accurate screening reports.